Hidden Costs of Denial Management in Medical Billing and How to Avoid Them
Medical billing is a complex process that involves submitting claims to insurance companies to receive payments for services rendered to patients. This process is essential for healthcare providers to maintain their financial stability and provide quality patient care. However, even with the best practices in place, denials are inevitable, which is why it is crucial to have a robust process of denial management in medical billing.
Denials occur when insurance companies refuse to pay for a service, which can be due to various reasons, including coding errors, insufficient documentation, or lack of medical necessity. Managing these denials can be a daunting task for healthcare providers, as it involves identifying the reason for denial, appealing the decision, and resubmitting the claim.
Understanding Denial Management
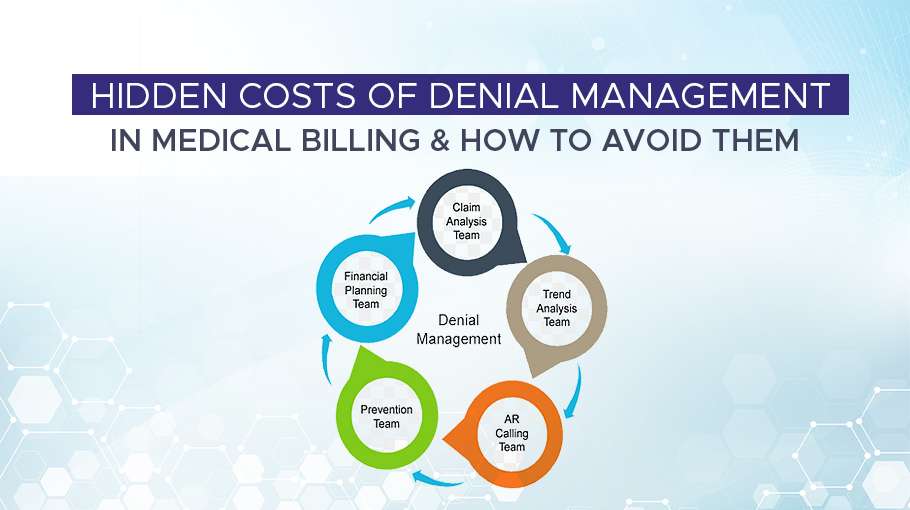
Denial management is a critical process in medical billing that involves identifying and resolving denied claims. Healthcare providers need to understand the root cause of denials, appeal the decisions, and implement best practices to prevent future occurrences. For medical billing company having a robust denial management process in place, providers can improve their financial health, streamline their revenue cycle management, and provide better patient care.
Medical billing is a complex process that involves submitting claims to insurance companies to receive payments for services rendered to patients. This process involves several steps, including verifying patient information, verifying insurance eligibility, coding the services provided, submitting claims, and receiving reimbursements.
However, even with the best practices in place, denials are inevitable. Denials occur when insurance companies reject a claim for reimbursement, citing reasons such as incorrect coding, lack of medical necessity, or missing documentation. Denials can have a significant impact on a healthcare provider's revenue cycle and financial stability.
Steps in Denial Management Process
To manage denials effectively, healthcare providers must have a robust denial management process in place. A robust denial management process involves several steps, including:
Identifying and Tracking Denials
Healthcare providers must identify and track denials to understand the reasons for the denials and the impact on their revenue cycle. Providers can use software tools to track and analyze their claims data to identify any trends in denials.
Analyzing Denials
Once denials are identified, providers must analyze the root cause of the denial, such as incorrect coding or missing documentation. This analysis can help providers make informed decisions on how to prevent future denials.
Appealing Denials
Providers must appeal denied claims promptly to receive the reimbursement they are entitled to. Appeals should include all necessary documentation and be submitted within the insurance company's specified timeline.
Communicating with Payers
Healthcare providers must establish open communication channels with payers to understand their claim adjudication policies, reimbursement rates, and any changes in regulations. This can help providers improve their claims submission process and avoid denials.
Continuously Improving Processes
Providers must continuously review and improve their denial management processes to reduce the occurrence of denials. This can include investing in staff training, upgrading technology, and implementing quality control processes.
Denial management is a crucial process in medical billing that helps healthcare providers maintain their financial stability and provide quality patient care. Providers must implement a robust denial management process to identify, analyze, and appeal denials promptly, communicate with payers effectively, and continuously improve their processes. By doing so, healthcare providers can reduce the impact of denials on their revenue cycle and improve their overall financial health.
Hidden Costs of Denial Management
Denial management is an essential process in medical billing that involves identifying and resolving denied claims. However, this process can come with hidden costs that can add up quickly if not addressed. Here are some of the hidden costs of denial management in medical billing:
Time and Labor Costs
Denial management requires a significant amount of time and labor, from identifying the cause of denials to appealing denied claims. Healthcare providers must assign staff to handle denial management, taking them away from other tasks, leading to decreased productivity. Providers may also need to hire additional staff to manage the denial management process, which can add to their labor costs.
Delayed or Lost Revenue
When claims are denied, providers are not reimbursed for services rendered, leading to delayed or lost revenue. This can lead to financial instability and decreased cash flow, making it difficult for providers to invest in their practices. The longer it takes to resolve a denied claim, the greater the impact on the provider's revenue cycle.
Increased Overhead Costs
Denial management can lead to increased overhead costs, including printing and mailing appeals, additional staffing, and software costs. Providers may also need to invest in data analytics tools to analyze their claims data and identify trends in denials. These costs can add up quickly, leading to increased expenses and decreased profitability.
Strained Relationships with Payers
Denial management can lead to strained relationships with payers, which can have a long-term impact on providers' revenue. When providers appeal denied claims, payers may view them as a high-risk provider, leading to increased scrutiny and decreased reimbursements. Strained relationships with payers can also lead to increased administrative burdens, such as increased documentation requirements and additional reviews.
How to Avoid Hidden Costs of Denial Management
Healthcare providers can minimize the hidden costs associated with denial management by implementing strategies that optimize their denial management processes. Here are some strategies that can help avoid the hidden costs of denial management:
Identify the Root Cause of Denials
Providers should analyze the cause of denials to determine the underlying issues, such as coding errors, incorrect patient information, or issues with medical necessity. Identifying the root cause of denials can help providers implement effective solutions to minimize the occurrence of denials.
Use Technology
Providers can leverage technology to streamline their denial management process. For instance, using automated software tools can help automate denial workflows, reduce manual labor, and increase productivity. Providers can also use data analytics tools to analyze their claims data and identify trends in denials.
Train Staff
Providers should invest in staff training to improve their knowledge of the denial management process. This training can help staff members identify the root cause of denials, improve coding accuracy, and improve communication with payers.
Monitor and Track Denials
Providers should monitor and track denials regularly to identify any patterns or trends in their denial rates. This can help providers make informed decisions on how to reduce denials and improve their denial management process.
Communicate with Payers
Providers should establish open communication channels with payers to understand their claim adjudication policies, reimbursement rates, and any changes in regulations. This can help providers improve their claims submission process and avoid denials.
By implementing these strategies, providers can minimize the hidden costs associated with denial management and improve their revenue cycle management. Providers can also consider outsourcing their denial management process to a third-party vendor, which can help them streamline their processes and reduce overhead costs.
Conclusion
In conclusion, denial management is an essential process in medical billing that healthcare providers must prioritize to maintain their financial stability and provide quality patient care. However, denial management can come with hidden costs that can have a significant impact on a provider's revenue cycle, such as time and labor costs, delayed or lost revenue, increased overhead costs, and strained relationships with payers. To avoid these hidden costs, providers can implement strategies such as identifying the root cause of denials, leveraging technology, investing in staff training, monitoring and tracking denials, and establishing open communication channels with payers. By doing so, providers can minimize the impact of denials on their revenue cycle, improve their financial health, and ultimately provide better patient care.